WHAT IS GLAUCOMA ?
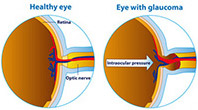
Glaucoma is an eye disease that causes loss of sight by damaging a part of the eye called the optic nerve. This nerve sends information from your eyes to your brain. When glaucoma damages your optic nerve, you begin to lose patches of vision, usually side vision (peripheral vision). Over time, glaucoma may also damage straight ahead (central) vision. You may not notice a loss of side vision until you have lost a great deal of your sight. When checking for glaucoma, eye doctors usually look for damage to the optic nerve and any loss of side vision. They may also check your eye pressure. Glaucoma is often called the ‘silent killer’ because people usually do not notice any signs of the disease until they have already lost significant vision. Once lost, vision cannot be restored.
WHAT ARE THE DIFFERENT TYPES OF GLAUCOMA?
There are many types of glaucoma. The most common types include:
- Chronic (Open Angle) Glaucoma:
This is the most common type. In open angle glaucoma, aqueous fluid drains too slowly and pressure inside the eye builds up. It usually results from aging of the drainage channel, which doesn’t work as well over time. However, younger people can also get this type of glaucoma. - Normal Tension Glaucoma:
This is a form of open angle glaucoma not related to high pressure. People with normal tension glaucoma may be unusually sensitive to normal levels of pressure. Reduced blood supply to the optic nerve may also play a role in normal tension glaucoma. - Acute (Angle Closure) Glaucoma:
Less than 10 percent of have this form, but It causes a sudden rise in pressure, requiring immediate, emergency medical care. The signs are usually serious and may include blurred vision, severe headaches, eye pain, nausea, vomiting or seeing rainbow-like halos around lights. Occasionally, the condition may be without symptoms; similar to open angle. - Secondary Glaucoma:
Another 10 percent of glaucoma cases come from certain diseases and conditions that damage the eye’s drainage system. These include diabetes, leukemia, and sickle-cell anemia also some forms of arthritis, cataracts, eye injuries or inflammation of the eye plus steroid drug use and growth of unhealthy blood vessels. - Post-Surgical Glaucoma:
which happen due to some surgeries, such as retinal reattachments increase the chance of getting glaucoma.
WHAT ARE THE THREE MAJOR SIGNS THAT A PERSON MAY HAVE GLAUCOMA?
- Optic nerve damage
- Vision loss (visual field loss)
- Increased eye pressure (elevated intraocular pressure).
Who is at Risk for Glaucoma?
These risk factors may increase your chance of having glaucoma:
Age:The older you are, the greater your risk
Race:African-Americans have glaucoma four to five times more often than others.
African -Americans: are also likely to have glaucoma at a younger age
Family history :If you have a parent, brother or sister with glaucoma, you are more likely to get glaucoma too. If you have glaucoma, your family members should get complete eye exams.
Medical history: Diabetes, previous eye injuries, eye surgery or long-term steroid use can increase your risk of glaucoma. Anyone can get glaucoma it affects one in 200 people until the age of 50. The rate increases to one in 10 over the age of 80.
What are the three major signs that a person may have glaucoma?
Optic nerve damage.
Vision loss (visual field loss).
Increased eye pressure (elevated intraocular pressure).
How Does Glaucoma Damage My Eyes?
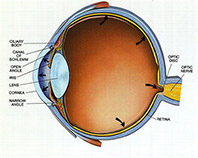
Your eye produces a watery fluid (aqueous humor), which goes into the eye and drains out.
When your eye is healthy, the fluid drains through a mesh-like pathway and into the bloodstream.
Aqueous fluid is produced by the ciliary body. It flows through the pupil and behind the clear cornea.
Finally, it drains away through the trabecular meshwork. For some people, fluid can’t drain properly because of a faulty drainage system.
Drainage that once worked well may gradually slow down as you get older. A sink that becomes clogged backs up with water.
When there is no place for excess fluid to go, pressure inside the eye builds up.
This increased eye pressure may damage the optic nerve over time. Slowly, the nerve fibers that are essential for vision die.
For others, glaucoma damages the optic nerve without increased pressure. These people may be unusually sensitive even to normal levels of pressure. Their glaucoma may also be related to problems with blood flow in the eye. Different people experience glaucoma differently.
Usually, glaucoma affects side vision (peripheral vision) first. Late in the disease, glaucoma may cause “tunnel vision.” In this condition, the person can only see straight ahead. That’s why someone with glaucoma can have good straight ahead (central) vision. However, even central vision can be seriously damaged.
Investigations
Tonometry: measures pressure in the eye. Medicine drops are used to numb the eye.
An instrument gently presses on the outside of your eye. Pressure is shown as a number followed by the abbreviation “mm Hg.” This stands for “millimeters of mercury,” a standard measure for pressure. An average pressure is about 16 mm Hg. Still, a higher than average number doesn’t always mean you have glaucoma.
Pachymetry: Thickness of the cornea (the front window of the eye) may affect the pressure reading and the risk of glaucoma progression, pachymetry is done to measure the same.
Ophthalmoscopy: few drops is placed in your eye to open or dilate the pupil. This allows the doctor a clearer view to inspect the optic nerve at the back of the eye.
Gonioscopy: After numbing the eye, the doctor gently places a special lens on the surface to examine the area in the front of the eye that drains fluid. Gonioscopy allows a more accurate diagnosis of the type of glaucoma.
Perimetry: evaluates your visual field. This tests your vision all around your field of viewing (360 degrees) to see if any areas are missing. It usually involves staring straight ahead at a light and trying to see lights that appear around the sides of your view. This is generally done with a computerized system.
Photography:or laser scanning may be used to show the appearance of the optic nerve inside your eye. This will also involve dilating your eye.
TREATMENTS: Glaucoma can usually be treated and controlled using medicine(s), laser surgery, glaucoma surgery or a combination of these treatments. Medicines (eye drops) are typically the first step in treatment, but laser surgery may be just as effective as a first choice. Your treatment is up to you and your doctor
Treating Glaucoma with Medicines: Doctors prescribe many types of medication to treat glaucoma. These drugs lower pressure inside the eye. Often, people with glaucoma have to take these medicines for life to control the pressure and limit vision loss.
OCT : Optical coherence tomography (OCT) is an imaging technique that uses coherent light to capture micrometer-resolution, two- and three-dimensional images from within optical scattering media (e.g., biological tissue). It is used for medical imaging and industrial nondestructive testing (NDT). Optical coherence tomography is based on low-coherence interferometry, typically employing near-infrared light. The use of relatively long wavelength light allows it to penetrate into the scattering medium. Confocal microscopy, another optical technique, typically penetrates less deeply into the sample but with higher resolution. Read More
Remember, you and your doctor must work together to determine the best medicines for you.
Treating Glaucoma with Laser Surgery
Some people may need eye surgery to control their glaucoma. Lasers are very useful for treating glaucoma because they avoid cutting and have a lower chance of complications (compared to glaucoma surgery).
There are three common laser procedures:
- Laser trabeculoplasty
- Peripheral iridectomy
- Laser cytophotometrically.
- Treating Glaucoma with Glaucoma Surgery
- Filtering surgery
- Drainage implant surgery
Filtering surgery
Creates a new path through the eye’s tissues to let fluid drain from the eye. In the most common filtering surgery, called a trabeculectomy, the surgeon makes a small opening in the white part of the eye (the sclera) to create a new outflow path. The fluid then flows through the new opening and creates a bleb, which is like a small bubble or reservoir on the surface of the eye. The bleb holds the fluid while it is slowly absorbed into the surrounding tissue. The upper eyelid usually hides the bleb, so it’s not noticeable to you or others. Most people who have this procedure no longer need medicine after surgery. Some people treated still need medicine, but they have better pressure control after the surgery. About 15 percent do not benefit from filtering surgery.
Drainage implant surgery
Drainage implant surgery is sometimes performed when a person is not suited for filtering surgery or when filtering surgery has failed. Depending on the kind of implant used, the surgery is called valve, shunt or seton surgery. In these procedures, the surgeon inserts a tiny tube through the sclera into the front part of the eye behind the iris. This tube becomes a path for fluid to drain away. The other end of the tube is attached to a tiny reservoir that acts like the bleb (described on page 19) to hold fluid until it is absorbed into the surrounding tissue. The reservoir is placed on the surface of the eye, back between the eye muscles, so it is not visible.
Risks of glaucoma surgery
A higher chance of getting cataracts.
Infection or leaking of the incision.
Adverse reactions to anesthesia.
What you do makes a difference
Remember to take notes and write down your questions so you can make the most of your doctor visit.
Explain to your eye doctor how the medicines are taking affect you.
Tell all your other doctors about your eye medicines and all other drugs you’re taking.
Read more about glaucoma and how to live with it.
Tell the eye doctor about any changes in your physical condition, any changes in your medicine or any side effects.
Getting more involved in your treatment
Even if surgery or drugs lower pressure in your eye, it’s still possible to lose vision. Therefore you and your doctor must carefully monitor the disease. Since you will be visiting your eye doctor regularly, take time and care in choosing a person who you are comfortable with. Your doctor should understand that your questions and concerns are important. A doctor who is willing to work with you, listen to your concerns and provide the best treatment plays a large part in your success against glaucoma. You may need medicines every day for the rest of your life. Find support and encouragement from your family, friends and others. Sometimes it helps to talk to people who have experienced the same thing. It can help you to discuss side effects, share ways to remember your medicines and New medicines are being developed and other treatments may soon become available. Promising scientific discoveries will help you look forward to a bright future.
Glaucoma FAQ